While the Tin Man in The Wizard of Oz (did you see the film Judy?) was not lacking courage, without a heart he would surely struggle to run away from the booming voice of The Great Oz. The Lion, on the other hand, had a heart and bearing in mind his lack of courage his ability to take fright and escape depended entirely upon his coronary circulation, the blood supply to his heart.
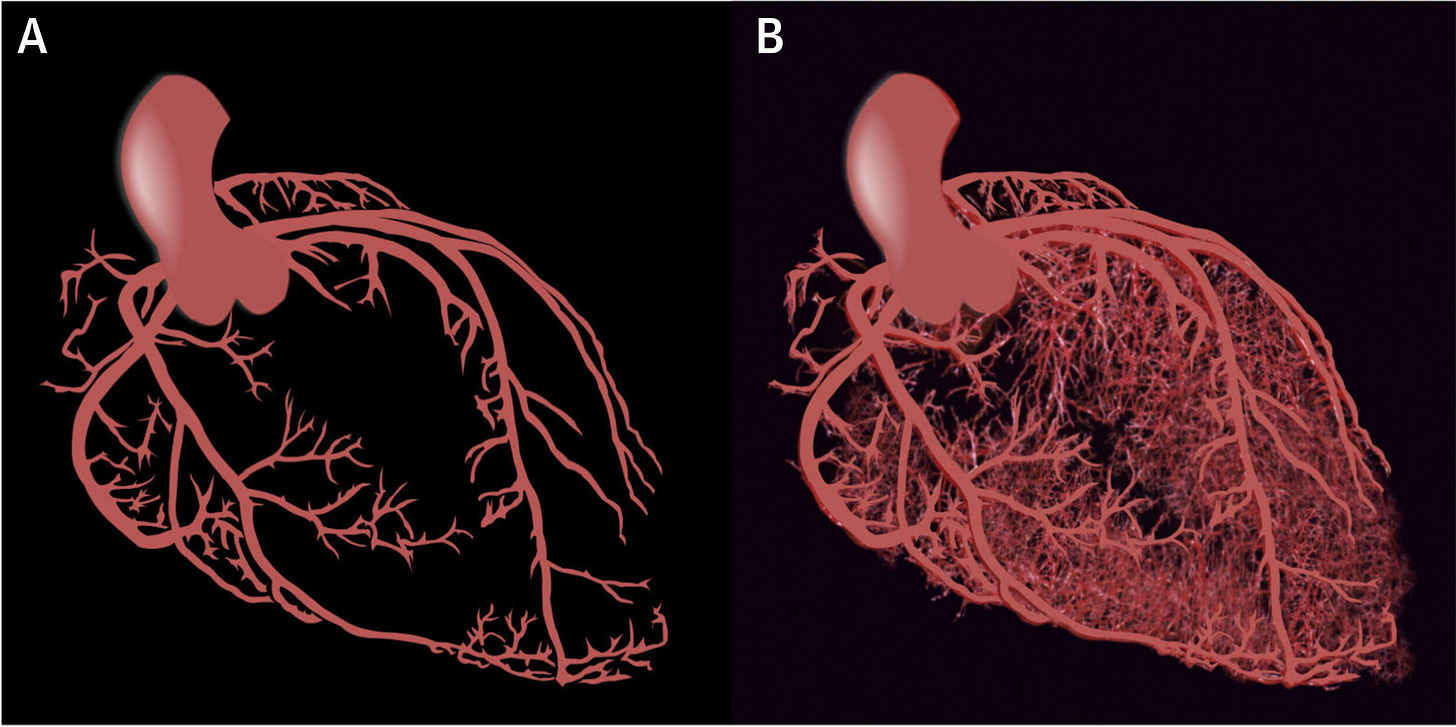
Consider the figure below..
On the left (A) is an image of the heart’s blood supply (coronary circulation) when the body and consequently the heart is at rest. While on the right (B) we have an example of what the coronary circulation might look like when you are being chased by someone with a large axe. The Tin Man?
When the heart is asked to work harder in pumping blood to the rest of the body the muscular heart cells are subjected to a much increased demand for energy. The energy currency is of course oxygen and this must be carried to as many heart cells as possible by the coronary circulation.
The increase in flow of blood to heart tissue shown in B is achieved by active dilation of existing blood vessels. The molecule that signals the vasodilation is ATP in the blood. I introduced ATP as an important extracellular signalling molecule in a previous post, see below.
Herein I want to write briefly about how we identified the mechanism whereby ATP brings about this remarkable effect.
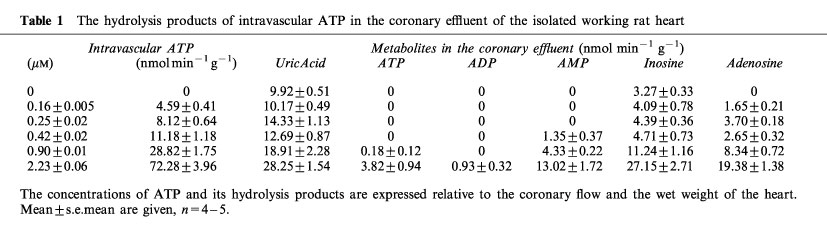
It is first important to appreciate that immediately upon its release into the bloodstream ATP is hydrolysed (broken down) by specific enzymes. We were able to measure this process in isolated rat hearts using a method called RP-HPLC. Some example data are shown below.
Our task was to identify which of the hydrolysis products of ATP was responsible for vasodilation of the coronary circulation. The enzymatic breakdown of ATP involves sequential removal of phosphate groups, so ATP is broken down to ADP which is broken down to AMP which is then broken down to give adenosine.
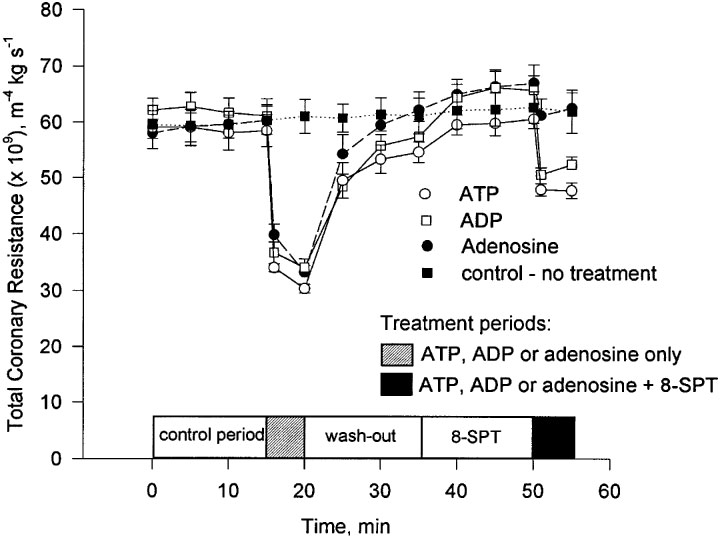
Previous research had suggested that adenosine was the main signalling molecule. However, when we blocked the activity of adenosine at its P1 receptor we only blocked half of the vasodilatory response. ATP and/or one of its immediate metabolites, i.e. ADP and AMP must also be responsible for the vasodilation.
This important observation is summarised in the below figure.
The figure shows that when the activity of adenosine is blocked using the pharmacological agent 8-SPT approximately half of the vasodilatory effect remains.
Further use of a number of pharmacological tools enabled us to identify that ADP and not ATP was responsible for the vasodilation and importantly that ADP mediated this effect through a specific receptor known as P2Y1.
We published these seminal finding in the British Journal of Pharmacology Research over the last thirty-five years has confirmed our observations and helped in the design and application of treatments for coronary heart disease.
However, I hear you cry, what has this got to do with aluminium. I will answer this by pointing out that you cannot understand a role for aluminium in coronary heart disease (CHD) without first understanding the mechanism that aluminium is most likely to interfere with, namely the activity of ATP as an extracellular signalling molecule.
We were able to address the role of aluminium in CHD in a number of follow-up experiments before the funding dried up. All further attempts to obtain funding for this research were denied. Plus ca change!




I pray often that there is a new day for ample funding for your brilliant research. Cheers to you Chris!
It's a curious thing, I have kidney damage from antibiotics administered while I had peritonitis as a child. Now in my 60s, protein loss had been gradually increasing until now. Several weeks into daily Si rich water consumption the dipstick colour change is diminishing.
It appears Al is highly nephrotoxic and just as it strangles brain neurons and glial cells, it must also impede kidney and liver neurons and their mutual neural communication.
Further, since this post focused on the heart, surely coronary neural networks are also poisoned.